Changing makeup of a specific protein has the potential to neutralize the virus
Researchers from McGill University are part of an international team led by the University of Buffalo, which has discovered a technique that could help increase the effectiveness of vaccines against SARS-CoV-2, the virus that causes COVID-19. The group’s study, titled “SARS-CoV-2 RBD Neutralizing Antibody Induction is Enhanced by Particulate Vaccination,” was published online in the journal Advanced Materials on October 28.
COVID-19 has caused a disruptive global pandemic, infecting at least 40 million and causing more than 1 million deaths worldwide. Since it began spreading in early 2020, biomedical researchers have been in active pursuit of an effective vaccine. Now, researchers suggest that one approach that may be effective is designing vaccines that partially mimic the structure of the virus.
“The most important contribution of this paper is that it opens a novel approach for the development of a COVID-19 vaccine,” says Prof. Joaquin Ortega, Professor in the Department of Anatomy and Cell Biology at McGill University and a co-author of the study. “We found that presenting one of the most important antigens in the SARS-CoV-2 virus, the receptor-binding domain (RBD), in the surface of nanodevices called liposomes induces a much stronger antibody response than when the RBD antigen is administered by itself,” explains Prof. Ortega, noting that liposomes are used extensively as nanodevices for drug delivery in cancer. “This paper shows that liposomes are also a unique platform for antigen presentation to the immune system and the development of effective vaccines.”
Importantly, the findings from this study creates a flexible COVID-19 vaccine development platform. The paper shows the new approach works efficiently when adsorbing the RBD antigen to the liposome’s surface. “However, the approach is, in principle, extendable to any other antigens from the Sars-CoV-2 virus,” notes Prof. Mike Strauss, Assistant Professor in the Department of Anatomy and Cell Biology at McGill, and a co-author on the paper. “We still do not know which of the viral antigens are causing the most robust immunity. Besides, specific antigens may generate adverse effects, including lung tissue damage, a significant issue encountered in the past during the attempts to develop vaccines against SARS-CoV-1 in the 2000s. Having a flexible platform for vaccine development, such as the one described in our paper, allows us to create ‘a-la-carte’ vaccines that only incorporate those antigens triggering a beneficial immune response but excluding those responsible for adverse effects.”
Leveraging McGill’s advanced microscopes for vaccine platform development
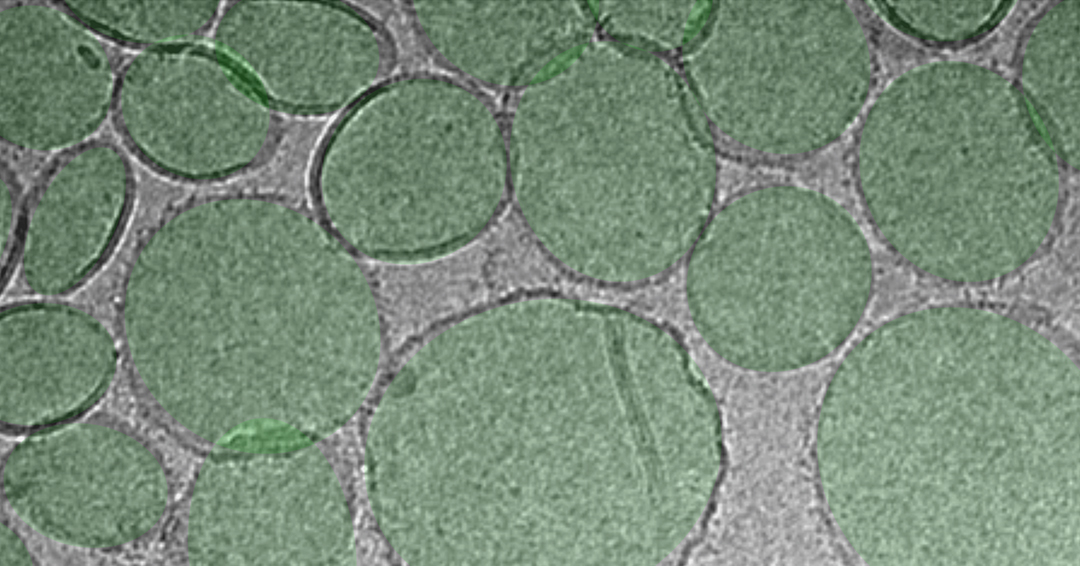
McGill’s contribution to this vaccine platform’s development was in the structural characterization of the nanoparticles used to deliver the antigen to the immune system, using the Facility for Electron Microscopy Research (FEMR) at McGill, the largest and most versatile cryo-electron microscope platform in Canada. This facility houses the most advanced and fastest electron microscopes in the world, producing extremely high resolution imaged that are essential for the characterization of nanoparticles, such as those used as antigen carriers in these vaccines. Cryo-electron microscopy images constitute the gold standard technique to ensure the liposomes carrying the antigens in the vaccine have the desired size and structure to induce a robust immune response.
Professors Strauss and Ortega, who are respectively the FEMR Technical Director and Scientific Director, loaded approximately three microlitres of the vaccine mixture into the Titan Krios microscope at FEMR. In the span of one hour, the Krios microscope produced over 300 images of the small lipidic vesicles contained on the vaccine. These images verified that the RBD antigen was being adsorbed in the lipidic surface of the liposome, which is the optimal location for antigen presentation to the immune system.
“FEMR cryo-electron microscopy images showing the structure and location of the RBD antigen in the surface of the lipidic vesicles was essential data for the development of this SARS-CoV-2 vaccine,” says Prof. Ortega. “There is no other method that allows for the direct visualization of the antigen adsorbed to the liposomes’ surface. Other biophysical methods can produce an indirect measurement suggesting the antigens may have been incorporated. Still, only cryo-electron microscopy is capable of visualizing these antigens on the surface of the liposomes directly.”
While the paper shows that this SARS-CoV-2 vaccine induces a robust immune response in mice animal models, the researchers say that like any other vaccine, it must undergo extensive additional testing and clinical trials before it can be administered to human communities. They also note that the evidence presented in this study that shows the RBD antigen benefits from being in particle format could help inform future vaccine design that targets this specific antigen.
Authors on the study include Jonathan Lovell, Wei-Chiao Huang, Shiqi Zhou, Xuedan He and Moustafa T. Mabrouk, all from the University of Buffalo Department of Biomedical Engineering; Kevin Chiem and Luis Martinez-Sobrido, both from Texas Biomedical Research Institute; Ruth H. Nissly, Ian M. Bird and Suresh V. Kuchipudi, all from the Animal Diagnostic Laboratory, Department of Veterinary and Biomedical Sciences at Pennsylvania State University; Mike Strauss and Joaquin Ortega from the Department of Anatomy and Cell Biology at McGill University; Suryaprakash Sambhara from the Immunology and Pathogenesis Branch of the U.S. Centers for Disease Control and Prevention; Elizabeth A. Wohlfert from the Department of Microbiology and Immunology at UB; and Bruce A. Davidson from the Department of Anesthesiology and the Department of Pathology and Anatomical Sciences at UB.
The study was supported by the U.S. National Institutes of Health, the McGill MI4 Interdisciplinary Initiative in Infection and Immunity, and the Facility for Electron Microscopy Research (FEMR) at McGill University. FEMR is supported by the Canadian Foundation for Innovation, Quebec Government and McGill University.
