The Graduate Certificate in Translational Biomedical Science Research aims to enrich basic science training through medical-style coursework and classes with health professionals
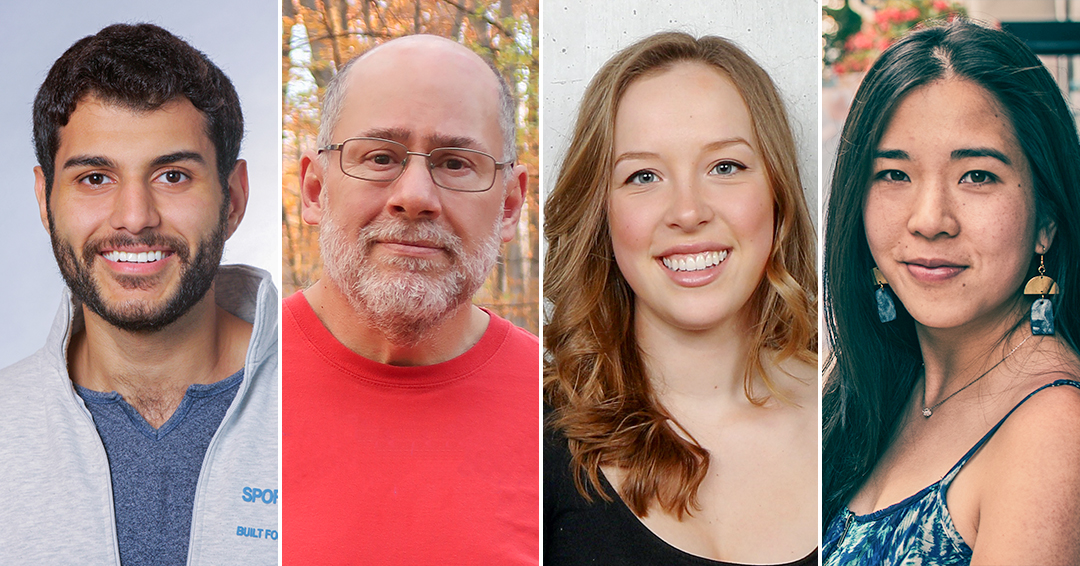
Since beginning his studies in biomedical sciences and neuroscience, Abdelrahman AlOkda, MSc, has worked towards one goal: ensuring his research has a concrete impact on people’s lives.
“We produce a lot of results in basic science labs, but many of these findings have no translation to real life,” the PhD student at McGill explains.
AlOkda, whose interests lie in developing interventions that promote healthy aging, then discovered a pathway to gaining the translational skills needed to achieve his aim: the Graduate Certificate in Translational Biomedical Science Research, offered by the Department of Pharmacology and Therapeutics within the School of Biomedical Sciences (SBMS).
Designed for current McGill graduate students in the science, technology, engineering and mathematics (STEM) fields, the program provides medical-style coursework, discussion-based classes with practicing clinicians and coursework that prepares students to design research projects with tangible clinical applications.
It was exactly the kind of experience that AlOkda had been looking for. He applied to be part of the first cohort, a group of 10 students who graduated earlier this year.
“The program was really invaluable, because it gave real-world context to our research,” he says. “Understanding clinicians’ perspectives and the challenges they faced helped us, as students, tailor our research questions and approaches to be more clinically relevant.”
Connecting with clinicians
The graduate certificate was first developed by Terry Hébert, PhD, Assistant Dean, Biomedical Science Education, and a group of students who were passionate about translational science.
Prof. Hébert recalls his own experience of learning about disease through an “idealized” lens in textbooks, which depicted patients as usually having only one health condition. By bringing in clinicians who can contextualize disease in the real world – where patients frequently have multiple conditions – the graduate certificate helps improve students’ understanding of clinical needs, he says.
“Getting to think about disease the way that clinicians do was eye-opening for the first cohort,” he adds. “It changes the way you frame out your next set of experiments. It changes the way you approach a problem when you’re coming up with a solution for a medical condition.”
Finding clinicians who had time to give a class on their specialty seemed daunting at first. But Prof. Hébert found the response from medical doctors was one of excitement.
“Everyone understood that this program fulfilled a deeply unmet curricular need by getting graduate students to think about problems in the way that health professionals think about them,” he says. “I could see that my clinical colleagues, who are used to thinking about the translational aspects of medicine, were really looking for this audience.”
Over the year-and-a-half long program, the cohort took lectures and tutorials in several medical specialties, where clinicians presented case studies and took questions from students about their work.
Sonya Hui, MD, a cardiology resident, taught in the cardiovascular block of the program – partly because she had previously completed a PhD in translational research.
“I remember what it was like to be in that position,” she says of the cohort. “Many of the students stayed late to ask me more questions and for career advice, since I had gone to graduate school before medical school.”
Peter Zylbergold, MDCM, MSc, a family physician based at St. Mary’s Hospital, presented anonymized cases from his work that covered a wide range of topic including cardiovascular health, mental health, care of the elderly, women’s health and the opioid crisis.
“The students were really engaged the whole time, he said. “They asked really good questions and put me on the spot in some ways.”
“I left with a good feeling inside, having done something different and perhaps shown the non-medical world a little bit of what we deal with on a daily basis.”
For AlOkda, the chance to have discussions, informal conversations and networking opportunities with clinicians was “just amazing”.
“This interdisciplinary approach really helped in understanding the practical challenges and opportunities that are associated with bringing all these scientific discoveries to the clinic,” he says.
Learning from each other
While Prof. Hébert led the rollout of the program, two of the learners who initially pitched it – PhD students Vivienne Smith and Charlotte Ouimet, MSc – helped out by auditing classes and organizing extracurricular activities.
At the career seminars, social events and networking trip to Harvard University they organized for the group, Smith and Ouimet observed the unique sense of community that the program helped to build among its students.
“Students told us that in grad school, you don’t really have a cohort. So, they really appreciated being with like-minded people who had unique experiences and who they could learn with and from,” says Ouimet.
Smith adds that the diversity of STEM fields represented in the cohort created a rich peer-learning environment for the students, one that could not easily be found in their own department where their peers normally had similar backgrounds or perspectives to them.
“There were people in biology, neuroscience, chemistry – all these different areas. That is really the heart of the program,” she adds. “It’s not just learning, mentorship or shadowing – it’s also the extracurricular career development from being immersed in a community of peer translational scientists that really lends itself well to the program.”
For AlOkda, highlights included a visit to the Steinberg Centre for Simulation and Interactive Learning (SCSIL) and an assignment that involved developing a translational research proposal.
“We needed to identify a clinical need, design a research strategy, and consider the regulatory and commercial aspects of our project,” he recalled. “It was then that I truly appreciated the complexity and importance of each step in the translational pipeline. There’s no point in finding a compound or drug that can be translated if you cannot advertise it and ensure it reaches the people who need it, or if it’s not going to be funded.”
Looking ahead to the next cohort – and beyond
After a successful run for the first cohort, applications are currently open for Winter 2025. However, Prof. Hébert has long-term plans for the graduate certificate’s future, including shaping it into a flagship program for the SBMS and seeking donor support for its growth.
“Students are going into a complicated scientific environment that requires them to think about the problems that patients have now, rather than about the pure, intellectual problem of studying a disease as a basic scientist,” he says, adding that the program helps break silos early on in their careers.
As he continues his PhD, AlOkda feels better equipped than ever to fulfil his dream of making a difference.
“My experience in this program has reinforced my desire to work at the intersection of research and clinical practice. I really hope that my work will have a tangible impact on patients,” he says.
“Although I’m not sure where I’d like to be yet, I know I want to have my research translated. I want to accelerate the translation of discoveries from bench to bedside – and back again.”
Students can apply for Winter 2025 cohort of the Graduate Certificate in Translational Biomedical Science Research until November 15, 2024. Learn more and apply.
Doctors, professors or prospective donors interested in being involved in the program can contact Prof. Hébert directly at terence.hebert@mcgill.ca.
Related:
New certificate program brings grad students and clinicians together

