The Neuro’s staff have been flexible and innovative during COVID-19
The COVID-19 pandemic has created unprecedented challenges for hospital staff around the world, and The Neuro is no exception. Staff have had to adapt to a rapidly changing environment, while protecting themselves and their patients from a serious disease.
 The measures put in place to stop COVID-19 start at the front door, where beginning in March everyone entering The Neuro has been screened for COVID-like symptoms. Security and staff evaluate people coming in for appointments and to work.
The measures put in place to stop COVID-19 start at the front door, where beginning in March everyone entering The Neuro has been screened for COVID-like symptoms. Security and staff evaluate people coming in for appointments and to work.They provide guidance on what to do if they show signs of the virus.
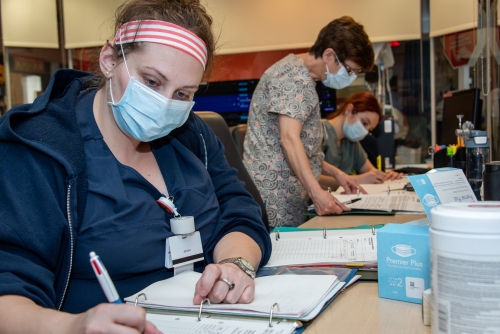
Outpatient appointments have been rescheduled and others are being changed to telephone appointments. Secretaries and administrative staff at The Neuro’s clinics are on the front line of providing information to patients and rescheduling appointments. “We had to increase communication among all of us,” says Viola Grasso, the coordinator of administrative services, Neuroscience Mission.
Innovation at the ICU
 While many elective surgeries have been postponed, The Neuro still receives stroke patients and performs emergency surgeries. The staff at the intensive care unit (ICU) have had to adapt their way of treating patients, to ensure proper care while minimizing the risk of COVID-19 transmission.
While many elective surgeries have been postponed, The Neuro still receives stroke patients and performs emergency surgeries. The staff at the intensive care unit (ICU) have had to adapt their way of treating patients, to ensure proper care while minimizing the risk of COVID-19 transmission.
Siva Moonsamy, nurse manager at the ICU, says the first challenge was assessing new information as it came in about the virus and what needed to be done to avoid spreading it. The management staff kicked into gear, adapting their procedures for the new reality.
One of the top priorities was creating negative pressure rooms so they could isolate patients who are suspected of having COVID-19. Staff are ready if patients test positive or develop symptoms while in their care.
 For some complex procedures, many health professionals must be present, yet a limited number of people are allowed in the negative pressure room with the patient at a given time. The ICU are solving this problem with video and audio equipment to communicate with medical staff outside the room.
For some complex procedures, many health professionals must be present, yet a limited number of people are allowed in the negative pressure room with the patient at a given time. The ICU are solving this problem with video and audio equipment to communicate with medical staff outside the room.The ICU team have also changed the way they stock crash carts, reducing the amount of medical supplies on them, because taking them in a room may expose them to the virus.
The team has created a new crash cart for emergency situations like a Code Blue and an intubation cart as well. These carts are stocked with the bare minimum to avoid contamination of medical supplies in the event the patient is COVID-19 positive. During a code, they keep these carts outside the room to reduce the risk of contamination. Moonsamy says fear of the virus was a problem at the start, but staff have overcome their fears to get the job done. They have also had help: a part-time nurse volunteered to work extra hours, a retired nurse came back and another from Doctors Without Borders joined the team.
Moonsamy says fear of the virus was a problem at the start, but staff have overcome their fears to get the job done. They have also had help: a part-time nurse volunteered to work extra hours, a retired nurse came back and another from Doctors Without Borders joined the team.
“This is the beauty of The Neuro,” says Moonsamy. “The sense of belonging to this institution.”
Changes in Neuroradiology
The neuroradiology department helps diagnose and treat abnormalities of the central and peripheral nervous system, spine, head and neck using neuroimaging.
The first challenge for the department was keeping up with protocols of how to deal with COVID-19. Cleaning medical imaging control stations and workspaces and managing inventory of personal protective equipment (PPE) to ensure proper dressing became critically important.
It also meant the staff had to adjust their isolation protocols for patient exams by either wearing PPE for procedures that may create potentially contaminated air particles or for exams with risk of contact with droplets.
The teams also had to differentiate between interventional procedures that create potentially contaminated particles suspended in air and those that do not. For example, normally after a CT scan detecting a stroke, patients are brought directly to the angiography suite. Now technologists along with the stroke team have developed a new patient pathway to allow intubation to be done in a negative pressure room to prevent disease spread. The collaborative efforts of different teams including technical services and anesthesia, allowed for the transformation of a room into a negative pressure work area suitable for intubation.
In the angiography suite the team installed plastic drapes to minimize potential exposure of staff as well as the specialized equipment within the suite.
“The entire medical imaging team continues every day to rise to the astounding challenge the pandemic brings forth,” says Julie Dumaine, manager of medical imaging at The Neuro. “It is amazing to observe the cohesion and solidarity among the staff. Strengths and talents are revealed.”
Dumaine gave the example of a neuroangiography nurse who helped produce a video of a simulation reviewing the workflow when a stroke patient with unknown COVID-19 status needs a CT scan and an angiography intervention. The entire team of medical imaging technologists, nurses, respiratory technologists, anesthetists and neuroradiologists worked together to find the best sequence of actions to minimize exposure and ensure best practices.
“The cohesive exercise was very educational for the entire team both professionally and personally,” she says.
May 14 2020




