By Diane Weidner, Steinberg Centre for Simulation and Interactive Learning
We all know that adopting a healthy lifestyle, including physical activity and sensible eating, is the best strategy to maintain a healthy weight. But sometimes life throws us off track, and for a myriad of reasons, the pounds add up. In 2017, according to Health Canada, 34 per cent of Canadian adults were overweight and 27 per cent were obese, with a body mass index (BMI) of 30 or higher.
Morbid obesity is defined as abnormally high BMI of 40 or higher. This serious health condition is associated with numerous chronic diseases, including diabetes, cardiovascular diseases and cancer. Severe obesity is not the result of a simple lack of self-control; it is a lot more complex than that.
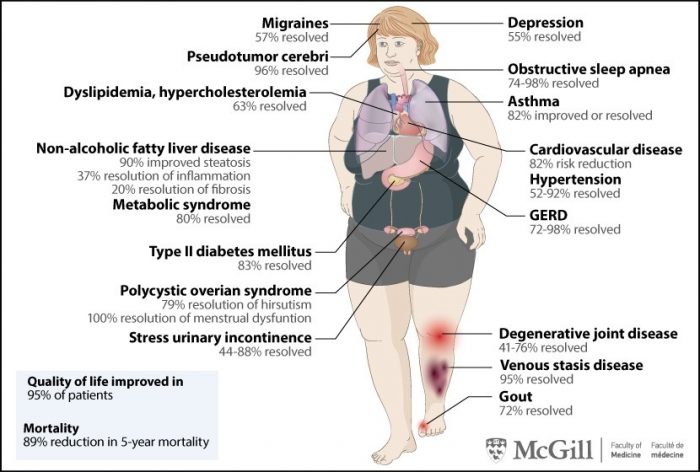
Dr. Zvi H. Perry is a bariatric surgeon who wants to raise awareness about the surgical treatment options for obese patients. “Obesity kills more people than guns around the world, with over 4 million deaths per year,” emphasizes Dr. Perry. “Almost any chronic disease has been associated with obesity. Over 70 per cent of people who suffer from type 2 diabetes are obese. And what about hypertension, cardiovascular disease, stroke, cancer, infertility, sleep apnea, psychosocial issues, varicose veins… I can go on and on.”
Dr. Perry came to McGill in 2017 to complete a one-year clinical fellowship in bariatric surgery, working with world-renowned surgeons at the Montreal General Hospital of the McGill University Health Centre (MUHC), including Dr. Olivier Court, Dr. Amin Andalib and Dr. Sebastian Demyttenaere. “I was really lucky to learn from such great mentors; to understand how, when and for whom bariatric surgery is appropriate,” says Dr. Perry. “Research has shown that the most sustainable way of treating morbid obesity in this day and age is through surgery. Yet only one per cent of the people who need it are given this option. There are huge benefits to be gained when patients undergo bariatric surgery. They can live longer and healthier lives. It’s truly life-changing. If an obese patient undergoes a bariatric procedure, s/he will add almost 10 years to her/his life expectancy.”
In the following diagram, one can see some of the proven benefits related to bariatric surgery.
Bariatric surgery has evolved
“Years ago, when bariatric surgery was performed through large incisions during open surgery, the success rates were lower and the complication rates were higher,” explains Dr. Perry. “People were fearful of the operation and associated it with pain and suffering. This has changed. The vast majority of bariatric surgery done today is performed laparoscopically using small cuts. It is minimally invasive, resulting in quicker recovery and a lot less complications.”
At the MUHC, there are three types of bariatric surgery performed laparoscopically: sleeve gastrectomy, roux en Y gastric bypass, and biliopancreatic diversion with duodenal switch. These procedures make the stomach smaller so that the patient will feel full faster and eat less, or cause malabsorption by rerouting the intestines, both resulting in gradual weight loss after the surgery. Patients who undergo bariatric surgery at the MUHC are well supported. They attend information sessions with a surgeon who describes the different types of surgery, a dietician who talks about what nutritional changes need to be made before and after the surgery, and a nurse practitioner who provides a timeline and practical tips. Other resources are offered to help support long-term changes to lifestyle and health, including consultations with a psychologist, physiotherapist, plastic surgeon, endocrinologist or other specialists depending on the patient’s needs. “When you have weight-loss surgery, you need a whole team involved. The patient needs to be monitored by specialists who will take care of them. We see superior long-term patient results with this team-based approach,” adds Dr. Perry.
In Quebec, weight-loss surgery is fully covered by RAMQ for eligible patients. This includes patients with a BMI over 40, or a BMI over 35 but with obesity related comorbidities, such as diabetes, sleep apnea, or high blood pressure. For more info: https://mcgill.ca/x/ZNq
Educating medical personnel who treat obesity
After completing his bariatric surgery fellowship, Dr. Perry stayed on to pursue a surgical simulation clinical fellowship at McGill’s Steinberg Centre for Simulation and Interactive Learning (SCSIL) with the goal of facilitating a structured educational program in bariatrics. “There is a growing need to better educate medical personnel who treat obesity,” he explains. “The approach to obese patients, the surgical evaluation and the post-operative treatment are poorly understood and studied. All health care professionals need to be better educated about their specific needs.”
Working closely with faculty and colleagues at the McGill Centre for Bariatric Surgery, the Department of Surgery, and the SCSIL, Dr. Perry performed a needs assessment to better understand what bariatric students, residents and fellows are being taught and to evaluate what educational methods best convey these needs.
For the past year, Dr. Perry has been working in collaboration with Dr. David Fleiszer and with Dr. Nancy Posel on a project supported by the McGill Molson Informatics Unit. Together, they have developed three virtual patients, one lecture and two cases to highlight the identification, diagnosis risk and initial treatment associated with morbid obesity. “I had great mentors who taught me that treating obese patients is very complex and necessitates team work, that it’s more important to be safe than to be quick. I want to give back and share this knowledge so that surgeons who operate on obese patients can do it efficiently and safely. The virtual patient does this in a way that is more engaging way than having to read a 400-page technical manual.”
Dr. Posel agrees whole-heartedly: “This innovative teaching strategy, based on the integration of virtual patients with the Simulation Centre (often referred to as blended learning) enriches, enhances and provides a more cost-effective approach to the teaching and learning in a digital age and expands valuable and existing resources.”
Dr. Perry’s goal is to apply this model at McGill and beyond, to be a part of real change and see tangible results and impact on the patient experience in places around the world that don’t have access to the resources and simulation expertise that are available here.
July 2 2019
