New guideline from the Canadian Task Force on Preventive Health Care
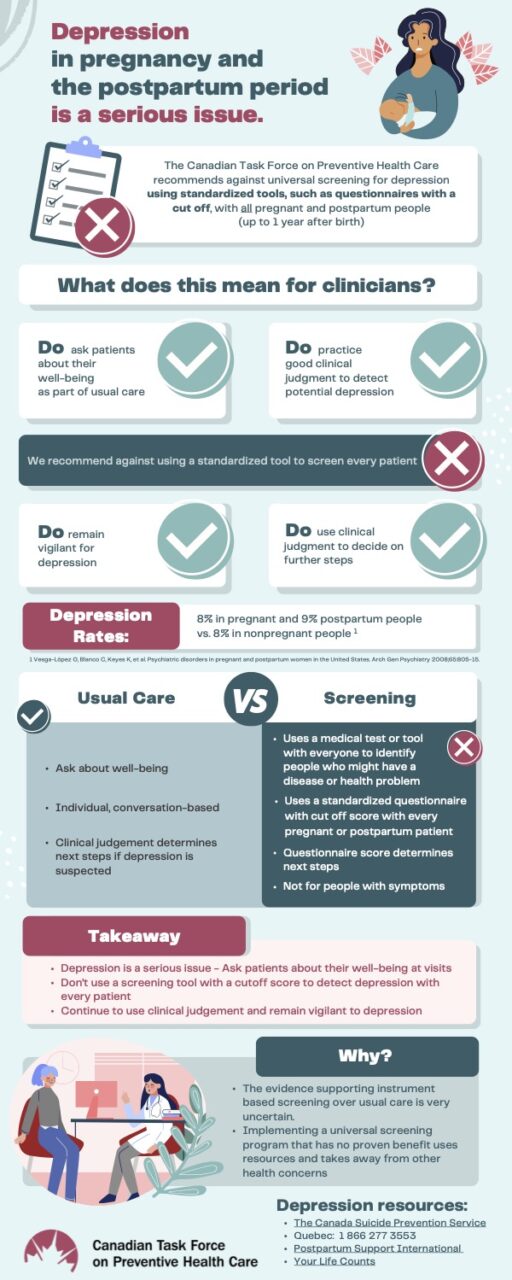
Depression in pregnant and postpartum people is a serious issue. Rather than using a screening tool with a cutoff score to detect depression in every pregnant and postpartum patient, clinicians should ask patients about their well-being as part of usual care, recommends a new guideline from the Canadian Task Force on Preventive Health Care published in CMAJ (Canadian Medical Association Journal).
“Depression in pregnant and postpartum people is devastating, with a massive burden for families and it’s critical to detect it,” says Dr. Eddy Lang, an emergency physician and professor, Cumming School of Medicine, University of Calgary and chair of the task force’s pregnancy and postpartum working group.
However, there is little evidence that universal screening for depression using a standard questionnaire and cutoff improves patient health, indicating more research is needed.
“We were disappointed to find insufficient evidence of benefit to universal screening with a questionnaire and cutoff score; rather, it’s best for primary care clinicians to focus on asking patients about their well-being at visits,” says Dr. Lang. “The emphasis is on an individualized approach rather than one-size-fits-all.”
Rates in pregnant people are about 8% and 9% in postpartum people compared with 8% in non-pregnant adults.
The task force engaged patients to understand their values and preferences to inform recommendations. Participants felt strongly that a discussion about depression with their health care provider during pregnancy and the postpartum period is critical.
- Physicians, nurses, midwives and other health care professionals in Canada with pregnant and postpartum patients.
- It applies to pregnant and post-partum people in the first year after delivery but not to those with a history of depression or being assessed or treated for other mental disorders.
- ask patients about their well-being as part of usual care
- consider not using a standardized tool with cutoff to screen every patient
- remain vigilant for depression
- use clinical judgment to decide on further steps
“Given the health implications of depression during this period, it’s essential to check in with people about how they’re feeling,” says task force member Dr. Emily McDonald, associate professor, McGill University and a physician at the McGill University Health Centre. “If clinicians are uncertain about how to start the conversation, they could refer to questionnaires for discussion prompts, which is different than formal screening that would use a cutoff score to determine next steps.”
As the practice of screening varies in Canada with several provinces and territories recommending screening using a standardized tool, updated guidance was needed.
“Jurisdictions that employ formal screening may wish to reconsider given the very uncertain evidence of benefit,” says task force member Dr. Brenda Wilson, a public health physician, professor at Memorial University, St. John’s, Newfoundland, and task force co-chair. “What’s essential is clinical vigilance for depression as part of usual care, as engaging in practices with no proven benefit can take away from other health issues.”
The College of Family Physicians of Canada has endorsed the guideline.
Get the guideline and related tools here.
If people are feeling down or depressed, speak to a primary care clinician or access a depression resource:
- The Canada Suicide Prevention Service
- Quebec: 1.866.277.3553
- Postpartum Support International
- Your Life Counts
The Canadian Task Force on Preventive Health Care is an independent panel of health experts in preventive health care and guideline methodology that develops evidence-based clinical practice guidelines for primary care.
SOURCE Canadian Task Force on Preventive Health Care
For further information: Media contact for interviews: Kim Barnhardt, media@canadiantaskforce.ca or kim.barnhardt@cmaj.ca