In a study published in Nature, RI-MUHC researchers examine how the lung copes with invading microbes
Every day humans breathe in about 11,000 litres of air, providing the oxygen required for life. However, breathing also allows microorganisms, particles, or pollutants access the lung. How does the lung adapt to various environmental challenges to ensure the elimination of invading microbes, while preserving its essential functions?
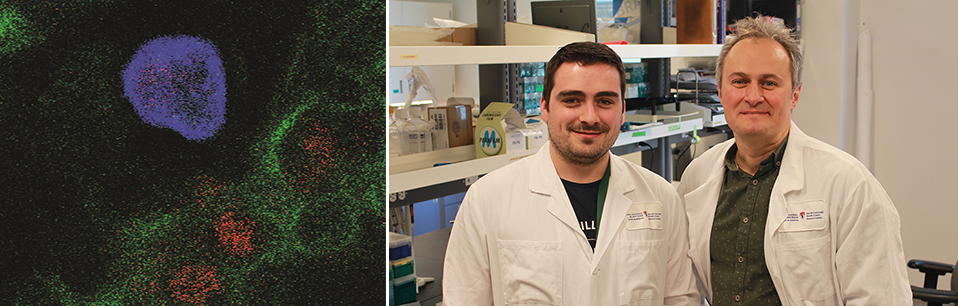
Recently published in Nature, researchers from the Research Institute of the McGill University Health Centre (RI-MUHC) investigated aspects of this question in their article entitled “Neonatal imprinting of alveolar macrophages via neutrophil-derived 12-HETE.” For the first time, the team was able to discern vital cellular and molecular mechanisms in embryonic development that ensure lung function throughout the life of an organism.
“As soon as we take the first breath of air, our lungs are populated with a unique subset of immune cells called alveolar macrophages (AM), which are constantly patrolling our airways,” says professor and senior author Maziar Divangahi, PhD, a pulmonary immunologist and senior scientist in the Translational Research in Respiratory Diseases Program at the RI-MUHC. “Alveolar macrophages play an important role in inducing immune responses to kill pathogens and inhibiting inflammation to limit damage to the lung.”
Although they are generated in the embryo, alveolar macrophages maintain their capacity for self-renewal and continue to protect the lung throughout life. How AMs can maintain this longevity was largely unknown until the publication of this study.
“Our laboratory has previously demonstrated how the functions of pulmonary macrophages like AMs are regulated in host defense against lung bacterial or viral infections,” says first author Erwan Pernet, a postdoctoral fellow with Professor Divangahi at the time of this study. “However, in this study, we were able to reveal the neonatal processes that shape the longevity of AMs.”
The research team focussed on the role of bioactive lipids called host lipid mediators. They were surprised to find that removing a lipid mediator called 12-HETE led to a significant reduction of AM numbers in adult lungs. Collaborator Jun Ding, PhD, of the RI-MUHC, conducted analysis of the transcriptomic profile, measuring RNA levels for genes in alveolar macrophages. This work revealed that 12-HETE is required for the self-proliferation of AM and prevention of AM senescence. With Bryan Yipp, MD, from the University of Calgary and Ajitha Thanabalasuriar, PhD, from McGill University’s School of Biomedical Sciences, the team then found that neonatal neutrophils were the major producer of 12-HETE and were required to maintain the proliferative capacities of AM. Then, collaborator Luis Barreiro, PhD, from the University of Chicago identified that epigenetic programming of neonatal AMs occurred via neutrophil-derived 12-HETE.
“Our results highlight the complexity of early life interactions between immune cells. Neutrophil-derived 12-HETE during early life is essential for the self-proliferation of alveolar macrophages,” says Professor Divangahi, who is the Strauss Chair in Respiratory Diseases as well as Professor of Medicine at McGill University, Associate Director of the Meakins-Christie Laboratories and Associate Director of the McGill International TB Centre. “The reduction of AM in aging individuals, who had increased susceptibility to pulmonary infection or inflammation, has tremendous clinical implications for immunity to infectious diseases and the lung health of an aging population.”
About the study:
Read the publication in Nature.
The authors gratefully acknowledge technical support from the RI-MUHC Histopathology platform, and funding support from the Canadian Institutes of Health Research, the Fonds de recherche du Quebec – Santé, and the Strauss Foundation.
