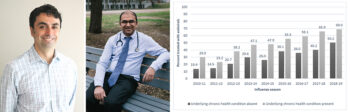
Dr. Jesse Papenburg and Dr. Kayur Mehta (L to R). Figure 3 from the publication shows the percentage of patients treated with antivirals across 12 Canadian IMPACT pediatric hospital centres by influenza season, 2010-2011 to 2018-2019 (n=7545), stratified by presence or absence of an underlying chronic health condition.
Findings show that influenza antivirals are underutilized in Canadian pediatric hospitals, despite national clinical practice guidelines
Published this month in Pediatrics, a new study by researchers from the Research Institute of the McGill University Health Centre (RI-MUHC) may lead to stricter adherence to influenza treatment guidelines and antimicrobial stewardship practices.
Led by Jesse Papenburg, MD, M.Sc., a senior scientist in the Infectious Diseases and Immunity in Global Health Program (IDIGH) at the RI-MUHC and a pediatric infectious disease specialist at the Montreal Children’s Hospital of the McGill University Health Centre (MUHC), this study found that influenza antivirals were underutilized among children hospitalized for influenza in Canadian pediatric hospitals.
“We decided to explore the extent and factors associated with antiviral use among Canadian children hospitalized with influenza in the decade following the 2009 H1N1 pandemic,” says Dr. Papenburg, who conducts research at the RI-MUHC’s Centre for Outcomes Research and Evaluation. “Observational studies suggest that early antiviral therapy in patients hospitalized with influenza is associated with improved outcomes; however, pediatric data are scarce. Despite guidelines recommending treatment, it is unknown why many children admitted to pediatric centres do not receive antivirals.”
“We found that antiviral use was limited and variable among Canadian children hospitalized for influenza. Over time, utilization increased overall and increased with high-risk children,” says Kayur Mehta, MD, M.Sc., a research fellow at the MUHC and first author of the study. “Our findings show that patient and hospital-level characteristics influenced antiviral use. Early antiviral initiation was strongly associated with rapidity of influenza test results.”
“These findings are important because they show that despite national clinical practice guidelines, there was wide variation in antiviral prescribing practices across the country, including among children with high-risk chronic health conditions,” says Dr. Papenburg. “Prescribing varied considerably across sites and increased over time.”
The research team performed active surveillance for laboratory-confirmed influenza hospitalizations among children aged 16 years or younger at 12 Canadian hospitals, from 2010-11 to 2018-19. Logistic regression analyses were used to identify factors associated with antiviral use.
This surveillance activity was conducted as part of the Canadian Immunization Monitoring Program Active (IMPACT), an ongoing national surveillance initiative managed by the Canadian Pediatric Society and conducted by the IMPACT network of pediatric investigators on behalf of the Public Health Agency of Canada’s Centre for Immunization and Respiratory Infectious Diseases.
“Our paper shows that multifaceted hospital-based interventions are warranted to strengthen adherence to influenza treatment guidelines and antimicrobial stewardship practices,” concludes Dr. Papenburg.
About the study:
Read the publication in Pediatrics.
Dr. Papenburg was supported by a Chercheur-boursier clinicien career award from the Fonds de Recherche du Québec—Santé. Dr. Mehta was supported by an Alan Ross Academic Bursary Award from the McGill Department of Pediatrics.
