“I never teach my pupils, I only attempt to provide the conditions in which they can learn.”
– Albert Einstein
Providing a safe environment in which students can learn is at the heart of inquiry-based learning (IBL), a pedagogical approach introduced at the Ingram School of Nursing in 2017 as part of its curriculum revisions. Through a process of self-directed learning, IBL strengthens the development of clinical reasoning.
“There are so many unknowns in clinical practice. IBL helps students develop the reflex of identifying the gaps in their knowledge, figuring out where to get the missing information, and knowing how to apply it,” says Professor Sanzone, Program Director of the BSc(N) who, along with Professor Jodi Tuck, co-led the integration of IBL across the School’s BSc(N), BNI and MSc(A)-N programs.
The IBL approach is radically different from the lecture-style of teaching that most students are accustomed to, and, as such, can be cause for anxiety at first. The approach involves scaffolding, with levels of increasing complexity introduced into each scenario as the course progresses.
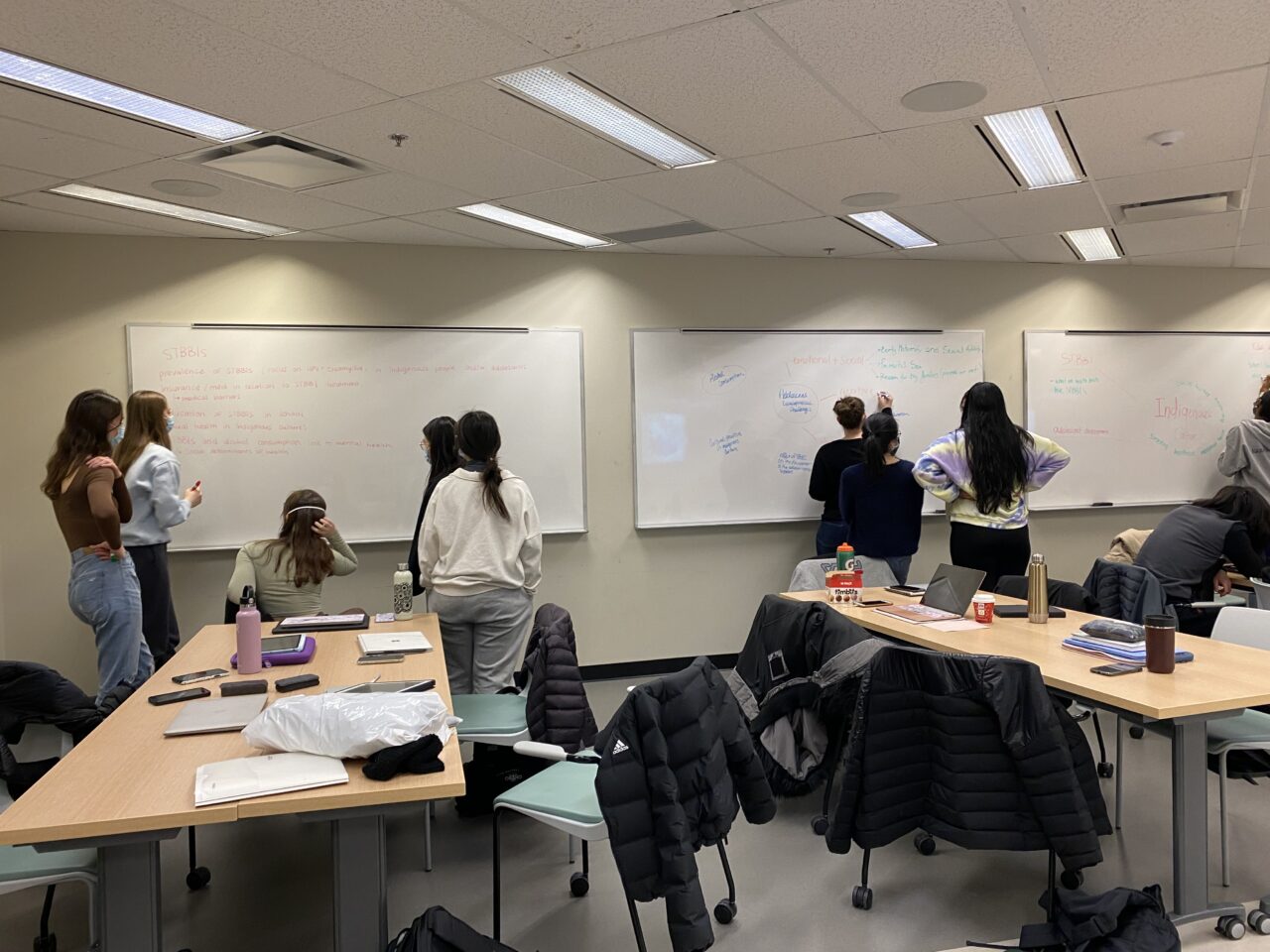
In the first phase, students are introduced to practice scenarios where they must determine “What do we know and what don’t we know?” They research the answers to these questions individually and then meet in small groups to share the evidence with each other and their classmates.
Phase 2 involves a simulation, where students develop therapeutic relationship skills with standardized patients. In the course of the simulation, the actors present the students with more unknowns and the students then make links between the evidence previously collected, the data observed or collected in the simulations and then repeat the process of gathering more evidence in regard to their new unknowns, allowing them to have a deeper understanding of the situation.
This allows the students to learn the necessary clinical reasoning skills in a safe learning environment, so they can develop the reflex to help them deal with multiple layers of complexity when caring for their patients and families in clinical settings.
Recognizing that nurses work as part of an inter-professional team, the IBL approach places a great deal of emphasis on helping students learn how to give and receive constructive feedback. At the end of each scenario, within their small groups, students give feedback to each other while assessing their own individual contributions to the team. They also debrief with the standardized patients who share how they felt during the scenario, highlighting which students’ approaches were effective and why. Finally, the facilitators debrief with the students as well, asking questions such as, “What was the rationale behind your intervention?” “What other ways could you have handled your interaction with the patient?”
IBL is challenging for professors as well. Rather than the traditional role of the “sage on the stage” who imparts information, the instructor acts as a facilitator, guiding the students’ learning. To ensure the successful implementation of IBL at the ISoN, Professors Tuck and Sanzone created a variety of faculty development tools including instructional resources such as videos, course templates, practice scenarios, facilitator guides, student assessments, policies and procedures, evidence based mapping documents and a two-day workshop on how to deliver the course content in a collaborative fashion. As well, ongoing Community of Practice meetings, held twice per term, provide facilitators with the opportunity to address any challenges they face, to evaluate and rework scenarios and to share new teaching strategies and initiatives.
In recognition of their successful implementation of this dynamic pedagogical approach, Lia Sanzone and Jodi Tuck received the 2020 Faculty Awards for Teaching Innovation from McGill’s Faculty of Medicine and Health Sciences
As for the students, while they may be anxious about IBL at the beginning, by the time they complete their final IBL course, they feel better prepared for the reality and the complexity of modern-day nursing, where clinical reasoning is paramount. “Nursing is a continuously evolving science,” says Professor Sanzone. “As a university, our mandate is to give our students the tools to become lifelong learners who promote evidence-based practice that enhances patient safety and quality of care.”