The Black Community Health Forum: Black Experiences in Healthcare, co-hosted by the Office of Social Accountability and Community Engagement (SACE), discussed concrete ways to improve care and services and increase representation in research, training and education
Advocating for her two-year-old son Isaiah following routine surgery to repair a hole in his heart in a Montreal hospital in 2001, Charlene Hunte encountered anti-Black discrimination at every turn. She shared her heart-rending story with attendees of the Black Community Healthcare Forum: Black Experiences in Healthcare, co-hosted by the Black Community Resource Centre (BCRC) and the Faculty of Medicine and Health Sciences’ Office of Social Accountability and Community Engagement (SACE) on January 17, 2024.
When Isaiah showed signs of an infection, Hunte – a former staff member of the Jewish General Hospital who now runs the Union United Church food bank – felt hospital staff brushed her concerns aside because she is Black. As Isaiah’s condition deteriorated, health professionals pressed Hunte to sign a consent to place him on a heart-lung machine, emphasizing how costly this would be to the hospital, something she suspected might not have been mentioned to mothers who didn’t look like her.
Tragically, Isaiah died shortly after. Hunte would eventually learn that he died of a preventable infection that had caused him immense suffering in his final days.
Several years later, Hunte would lose her elder son Andrew when he was shot while trying to break up a fight. Her distressing dealings with the hospital where he received treatment confirmed that she and her family were treated differently because of the colour of their skin.
Attendee Farhan Bhanji, MD, Vice-Dean, Education, later told the group that he had heard about Isaiah’s case as a medical anomaly while training in pediatric intensive care, and was dismayed to hear the full story, which he and other learners hadn’t been told.
Trying to root out the kind of systemic racism Hunte faced in our healthcare system was one of the aims of the all-day forum, which was attended by members of Montreal’s Black communities, health professionals, students and members of the FMHS.
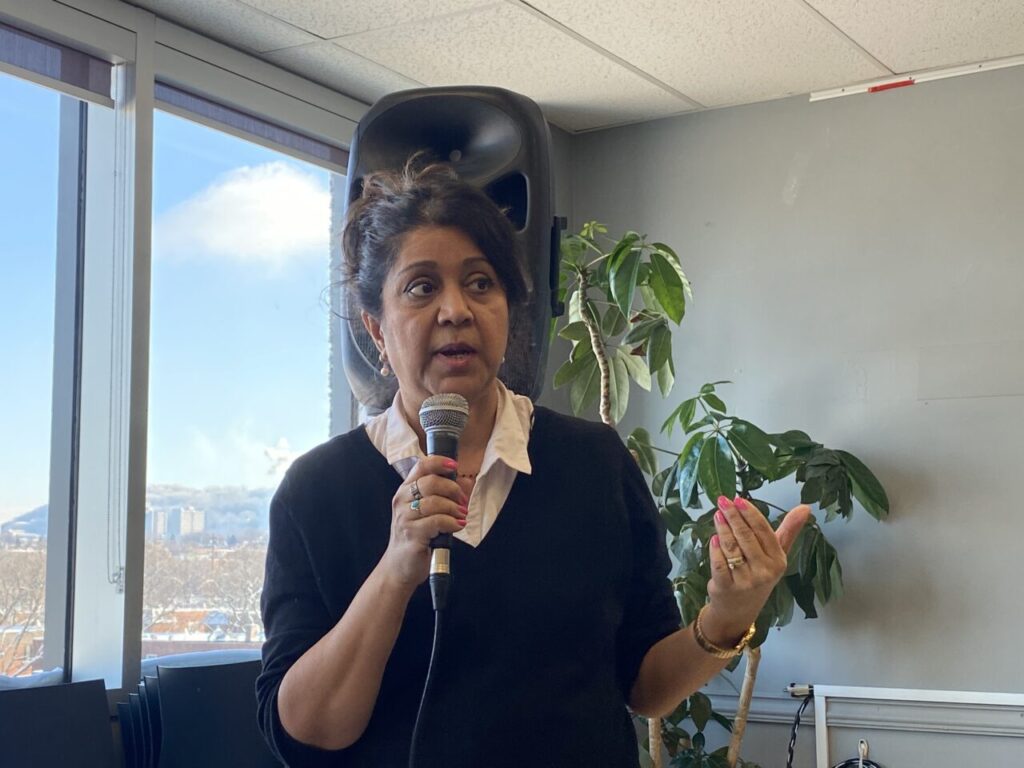
”We want to listen to the community and identify the barriers to living a whole, healthy life where your well-being is protected and supported,” said Baijayanta Mukhopadhyay, MDCM, Director of SACE. “Our job as a Faculty is to bring that reality more into being. We want to make sure our training, research and services are actually responding to the needs you express.”
Discrimination, bias leading to mistrust
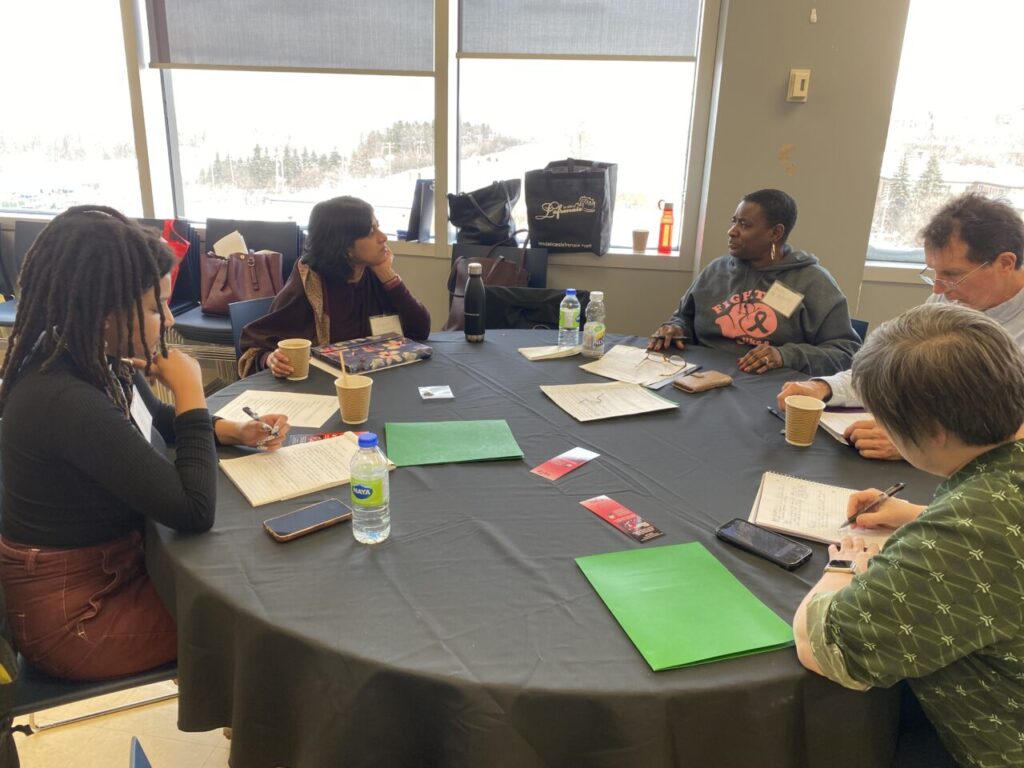
During a small group session, when asked about the barriers they experience in accessing healthcare, many Black community members reported that, like Hunte, they are often not taken seriously by health professionals. Others shared stories of health professionals failing to diagnose conditions like blood clots in Black patients, as they had less knowledge of how the symptoms appeared in non-white skin.
One group said they frequently experience discrimination when interacting with the health system based on their skin tone or their neighbourhood, affecting the quality of care they receive. This discrimination also creates a burden on Black health providers to advocate for Black patients and educate their non-Black colleagues, said Evelyn Ford, a retired Black nurse.
All this leads to a lack of trust in the health system among many Black patients, attendees agreed, which discourages them from seeking care until their symptoms are severe.
Greater representation and engagement with communities
Attendees were asked to come up with measurable improvements they would like to see in three areas: care and services, research, and training and education.
For care and services, many called for greater representation of Black people in the health professions.
“There are a lot of Black nurses and an increasing number of Black MDs, but not in positions of authority where the decision-making happens,” Mabel Carabali, MD, PhD, Assistant Professor in the School of Population and Global Health, noted via Zoom when reporting her virtual group’s thoughts. Dr. Carabali cautioned we have to “avoid burnout of these people – there are so few, they get called on a lot.”
Gemma Raeburn-Baynes, President of the GemStar Circle of Excellence Scholarship Program for Black students, noted she’s seen a positive difference in her care since getting a Black physician. Her fellow GemStar volunteer and teacher Latoya Belfon agreed, adding she felt a Black doctor understood her reality better. First-year medical student Khatra Badreldin couldn’t relate: “I have never had a Black healthcare provider,” she lamented.
One group recommended the establishment of an independent liaison to advocate for and help Black patients and others navigate the system in a culturally safe way, as well as an ombudsman onsite to take complaints in real time.
Dr. Mukhopadhyay also raised the issue of a lack of research on the specific health needs of Black communities, with another attendee commenting that this absence “invisibilizes their experience.” Others noted that such data is necessary to successfully advocate for policy change in healthcare.
John Davids, Research Coordinator at the BCRC, highlighted the need for community members to be on research committees to ensure questions are relevant to their experiences and that data is collected and managed securely. “These communities must have a space on committees – there are huge human rights and legal aspects that we don’t talk about,” he said. Seeta Ramdass, Associate Director of SACE, agreed, noting that Black committee members often quit in frustration because they feel their input is dismissed.
Although the value of measuring patient satisfaction was recognized by attendees, many said they failed to reach those who do not access healthcare, with Dr. Carabali noting: “When we measure levels of satisfaction if we only ask those who use the healthcare system, there will be a bias because we miss those who are not accessing healthcare and we need to find out why.”
Tanya Matthews, PhD, a postdoctoral research fellow in the School of Communication Sciences and Disorders who studies health literacy in Black communities, said she has noticed firsthand the value of having better representation of Black researchers, noting that families she visits are more comfortable opening up to her: “It’s because I look like them.”
In training and education, attendees noted that Black children are pushed away from science, technology, engineering and mathematics (STEM) streams as early as their elementary school education, potentially depriving them of careers in medicine, health professions or other sciences. Davids noted: “The legacy of anti-Black racism drags Black students away from these fields of study. Understanding this legacy helps us move on. We must acknowledge the harm done and only then can we repair the relationship.”
Attendees also supported increased recruitment of Black learners in medicine and health professions, and highlighted the need to ensure those learners feel that they belong in those institutions. Revising medical and health professions curricula to include more community engagement and to educate learners on empathy, racism and unconscious bias was also identified as a priority.
Powerful narratives for change
As the forum drew to a close, Dr. Mukhopadhyay and Ms. Ramdass thanked attendees and pledged to organize a follow-up event with the Black community within a year. Before then, SACE plans to write a report on the barriers and recommendations discussed at the forum. As Ms. Ramdass explained, speaking after the event: “This was a Black community-led initiative from concept to conclusion. The community decided the nature of the questions, the format for the forum, and even the final report will be achieved with community input and approval. This is part of our commitment to respect the community’s role in its own data governance, from collection to interpretation and reporting in a socioculturally safe and responsible manner.”
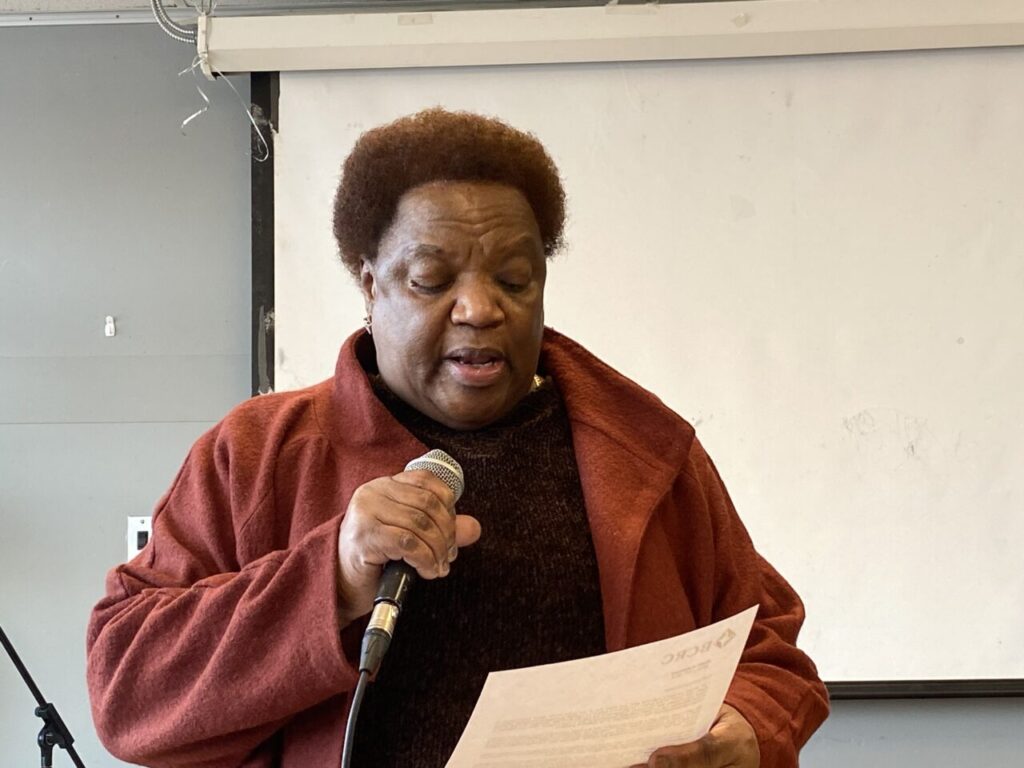
Yvonne Sam, a retired nurse and Chair of the Rights and Freedom Committee of the Black Community Resource Centre, also thanked attendees and remarked: “Today, we are here not only to share our stories, but be agents of change.”
“Our narratives are powerful. They shed light on lived realities that statistics alone cannot capture,” she added. “They compel empathy and drive change towards a more just and inclusive healthcare system.”
SACE acknowledges the support of Dr. Richard Koestner of the Human Motivation Lab at McGill University in providing funding this event.
- Charlene Hunte, with a photo of her son Isaiah behind her.
- Charlene Hunte shares her story
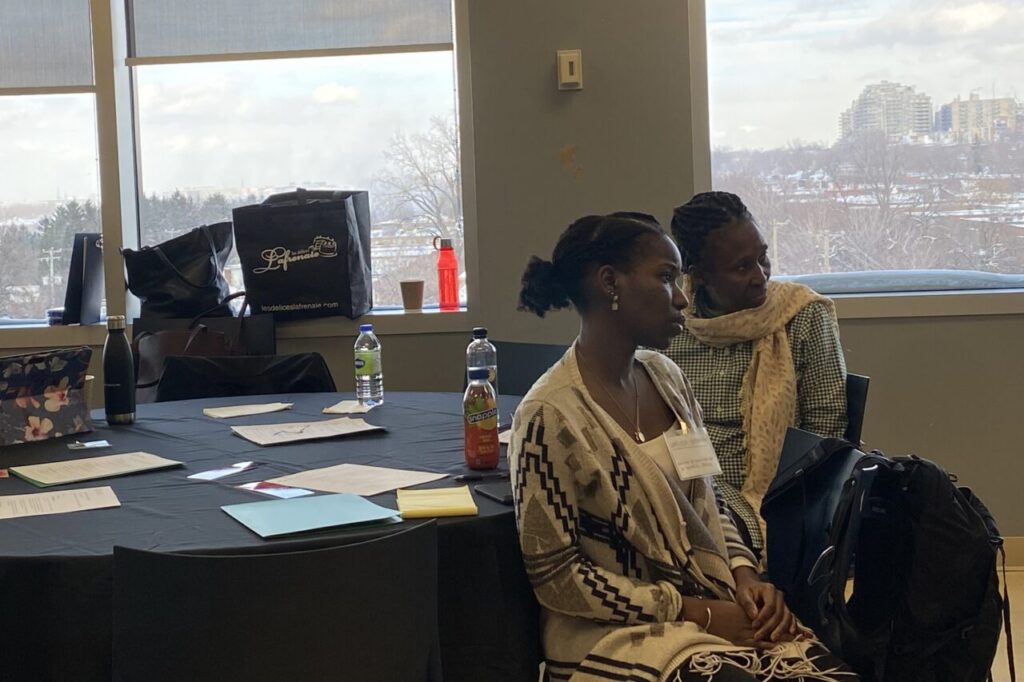
- Delegates listen to Hunte
- Seeta Ramdass
- Baijayanta Mukhopadhyay
- Yvonne Sam
- Medical student Khatra Badreldin
- Discussion group at the forum
- Break time.
- Baijayanta Mukhopadhyay moderates the discussion
- Small group discussion (Photo: Seeta Ramdass)
Related:
Experts want to know why Black people are still facing inequity in health care (Global News)